I was recently talking to a friend who mentioned that she was PMSing. In a few days, she’d gotten super angry, had a conflict with her boss, and fought with her boyfriend—and she saw it as a good thing. She talked about how the feelings of rage showed her where she needed to set boundaries and how difficult it was for her to say things to her boss that a man probably wouldn’t have thought twice about. “You just need to get over the rage part first,” she explained while chewing on the snacks she had bought for her son.
We usually look at PMS symptoms as something that can only be negative. I don’t think I’ve ever heard food cravings, irritability, and mood swings described positively. And, of course, when the symptoms get to PMDD level (meaning they cause significant distress or disruption to one’s life), it’s even harder to see any positives.
When I was really struggling and feeling hopeless about my ADHD, I detested it when people said things like “ADHD is a superpower.” It definitely wasn’t a superpower for me - I felt disabled by it. Yet learning about my hormonal cycle and working with IFS helped me recognize the possible benefits of the luteal phase, and as a result, my symptoms became less debilitating.
Our two (or more) selves
Women who report PMS express concern about losing control over their emotions and experiencing a "normal" compared to a "PMS" self.12
If you go on forums and groups for PMDD, you’ll see regular posts asking, “Which one is really me?”Often, women choose to see the “PMS-self” as “not them,” while the follicular self is easier to like: energetic, motivated, patient, kind…
It’s harder to like PMS-self when she appears angry, insecure, demanding, or needy. PMDD can cause severe disruptions to one’s life, including interpersonal conflict, impairment of daily functioning, and decreased enjoyment of hobbies and everyday activities. How can you love someone or something that’s ruining your life?
Internal Family Systems for PMDD
Internal Family Systems is a therapeutic approach developed by Richard C. Schwartz in the 1980s. It’s super trendy right now, particularly for issues such as complex trauma, addictions, and eating disorders. While I couldn’t find any studies about using IFS to treat PMDD, I’m going to argue that it can be beneficial, based on personal experience + studies that show that IFS was beneficial to things that relate to certain aspects of PMDD or moderate/severe PMS.
Disclaimer: I am not claiming that IFS, or any other approach, will “heal” you or get rid of all your symptoms. I am sharing one thing out of many that helped me.
What I did find is someone offering a webinar about IFS for suicidal parts in the luteal phase and a website claiming a case study of a woman who healed PMS/PMDD with non-IFS parts-focused psychotherapy. IFS is not the only way to do “parts work,” but it’s one of the main ways people talk about it today.
What is Internal Family Systems?
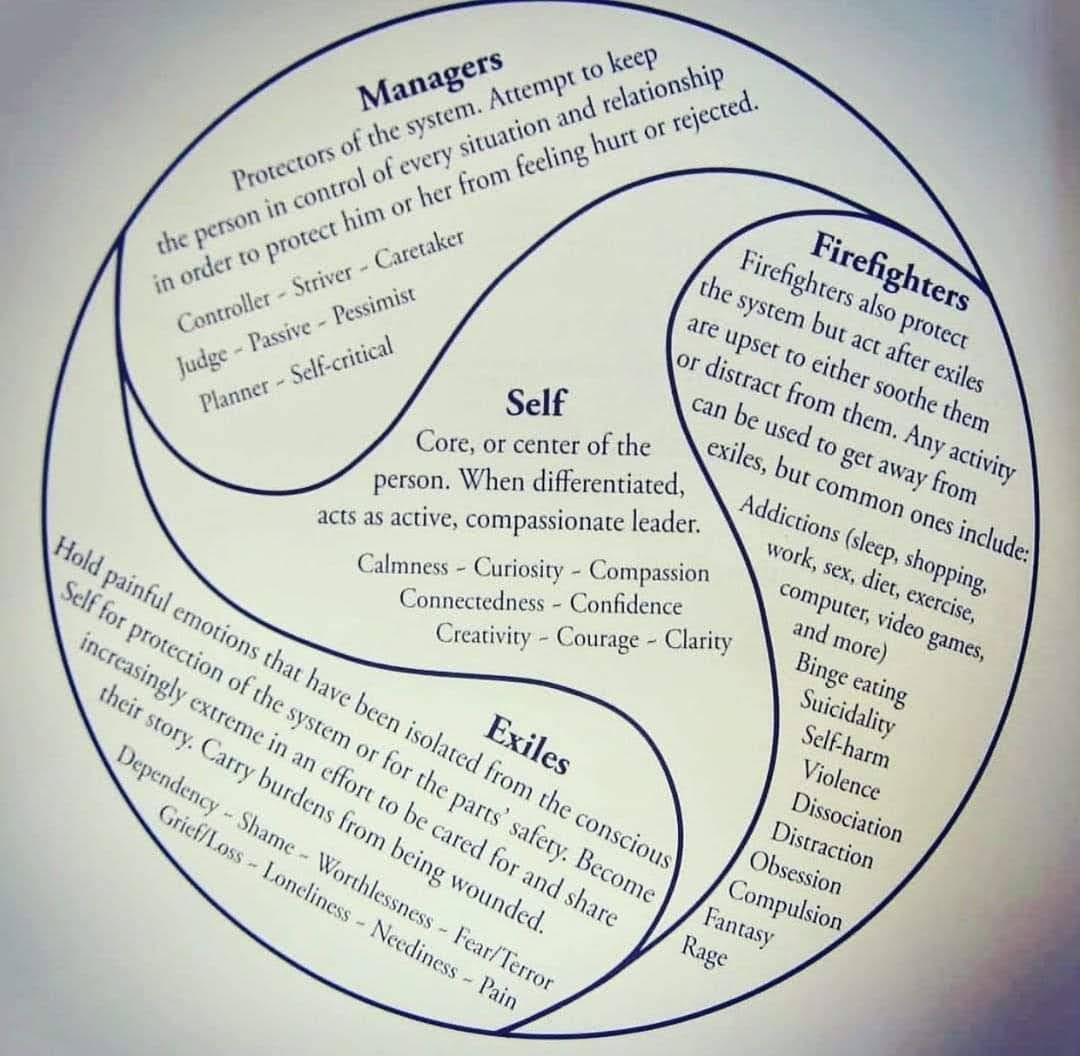
The basic tenet of IFS is that we’re all made up of “parts,” and all these parts have the same goal of protecting us, even if they have opposing ways of doing so and end up fighting quite a lot.
While these parts can take on extreme roles (such as substance abuse and other potentially harmful coping mechanisms or behaviors) due to trauma and other life circumstances, the parts themselves aren’t bad. Nor are they only there due to trauma and will automatically disappear once we “release our trauma.” In IFS, they use the term “unburdening” to describe the process of a part releasing something they’re holding on to.
I’ll be honest: I’m not 100% behind everything being said about IFS, but I think that’s just a consequence of any modality being in the public eye. We've seen it with CBT, psychedelic-assisted therapy, and other approaches throughout history; people get super into them, treat it as a panacea for everything, and it can get pretty culty-feely. Some modalities stick around, and some don’t as much. But I do believe parts work, whether IFS or others, can help work through PMS/PMDD symptoms.
Why use Internal Family Systems for PMDD?
IFS is a great model for working through trauma, and PMDD is highly correlated with trauma.
Studies show that women with PMDD do not differ in hormone levels from women who do not have PMDD, which indicates that the problem is not the hormonal fluctuations but the woman’s response to them3.
A bunch of studies show links between trauma and PMDD, including one that found that 83% percent of women with PMDD had experienced early life trauma, with emotional abuse being the most common at 71%4. The prevalence of emotional abuse was 61.9% higher in the PMDD sample than in the general Australian population.
Also, the prevalence of PMDD varies by country: 40% of Egyptian women surveyed, 34.7% in Jordan, and 28.2% in Syria, with a significant association between the frequency of experienced sexual harassment and the frequency of premenstrual symptoms.5 A meta-analysis estimated the worldwide prevalence of PMS at 48%, with a wide variance between countries, from 10% in Switzerland to 98% in Iran.6
There are a whole host of studies and books about trauma and IFS.
IFS can help recognize “follicular selves” and “luteal selves” as partners on the same team who need to learn how to communicate.
When we start to see the different parts of ourselves as wanting the best for us, they don’t need to be as loud.
The classic example is of a toddler who wants something, say a snack. They may initially turn to a caregiver for help, but if ignored, they’ll opt for a different strategy. They may have a tantrum, go and get the snack themselves (possibly making a mess in the kitchen), or steal another kid’s snack. Their desire for a snack didn’t disappear because it was ignored; it just got louder.
Things get rough when parts fight: Your exhausted part wants to rest, but another part says, “There’s too much to do, and a few days ago, it was fine. " So the exhausted part will get “louder,” making you feel like you can’t get out of bed if it’s the only way you can rest. But they can find better solutions if these parts communicate and work together.
IFS can work with biological conditions
While I haven’t found much (yet) about IFS and PMS/PMDD, there is acknowledgment and discussion of how parts work with biological conditions.
Transcending Trauma by Frank Anderson: “Parts and biological conditions have a strong relationship with each other. As Dick Schwartz often says, parts can push the biological button. My parts were telling me: “We caused the asthma attack to get your attention because you are not speaking up.” And the reverse is also true. Biological conditions can often affect parts, causing them to say: “This isn’t us—we have nothing to do with the asthma attack. It’s the winter, the heat is on, the air is dry, and you’re allergic to dust.” At other times, it’s a combination of both parts and biology, where they share a percentage of the responsibility. All we have to do is ask; parts are usually willing to help sort things out.”
Your angry luteal part may not be as crazy as you think; perhaps what seems to be picking random fights or blowing things way out of proportion is a response to things that bother you in your relationship all along, but you’ve been suppressing to keep the peace. Even if the feelings are out-of-proportion to what’s happening in the present, it can be a good sign that it’s bringing up something from the past that needs to be worked through.
IFS integrates well with other therapeutic modalities.
IFS can work with other modalities that can be beneficial for PMS/PMDD and the various conditions that it is highly comorbid with. Examples include creative and expressive arts therapies7, EMDR, somatic-based therapies such as Somatic experiencing, and person-centered counseling.
You don’t have to follow the “IFS manual” step-by-step (I don’t) to benefit from the framework and language (I do!).
Other therapeutic interventions have shown promising results.
While the majority of PMDD treatment research seems to focus on pharmaceutical interventions, this study on Emotion-focused therapy for women with PMDD found a decrease in PMDD symptoms such as depression, anxiety, and emotional dysregulation.8
There are a few other studies about different therapeutic approaches for PMDD, which I haven’t looked deeply into yet. But it makes sense that doing emotional work will help the emotional symptoms of PMDD, like irritability, anxiety, and mood swings. Various types of therapy can help with emotional regulation skills, deeper self-insight, and developing healthier coping skills.
How would IFS work with PMS/PMDD parts?
If you’re already tracking your cycle, you should start getting familiar with your patterns, even if they’re not 100% consistent month to month. Maybe you get a part that’s telling you that you should quit your job and move to the woods; perhaps it’s not letting you get out of bed; maybe it’s convincing you that your partner is cheating on you.
Arguing with these parts and explaining why they’re wrong doesn’t help (“but I need this job”; “they’re a loving partner, and you’re just imagining things”). Parts can argue back and be very convincing, so you go around in circles or what’s referred to as polarization in IFS terms. One team comprises parts that want you to protect yourself by isolating yourself, while team B wants you to be a functioning member of society. And neither is willing to give up their position.
Once you identify these parts and stop fighting them, you can learn more about what they need and are asking for. As part of my attempt to arrange my life more in sync with my cycle, I spend more alone time during luteal - and I found that I am more creative during this time. I may be on the floor thinking, but I have more ideas for projects and do more writing - and giving space for the tears to come up helps me release the stress from my busier follicular times and make adjustments to my life. I’m clearer on boundaries I need to set and things I want to communicate, more likely to do organization tasks, and overall, my life seems to be better because it’s not just one person or part trying to run the show and suppress other team members - there’s actual cooperation happening. As a result, I’m less stressed, and my symptoms aren’t as extreme.

Further reading and practical tips
Book: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard Schwartz
This is one of the two books on IFS I see most often recommended, but I haven’t read the other (Self-Therapy by Jay Earley).
Podcasts and videos
Podcast: IFS Talks
The podcast is geared mainly towards IFS therapists, but some episodes would be helpful for anyone who wants to use the model in their personal life.
Hebrew podcast about IFS: העולם בפנים
The podcast provides a good, structured, in-depth explanation of the IFS model and later features a demonstration. Unfortunately, due to the language, it is not accessible to everyone.
The first part is a series of videos that introduce and explain the IFS model and discuss the neuroscience behind it.
This three-part series addresses shame from an IFS viewpoint and ends with a guided meditation.
Chrisler, J. C., Gorman, J. A., & Streckfuss, L. (2014). Self-Silencing, Perfectionism, Dualistic Discourse, Loss of Control, and the Experience of Premenstrual Syndrome. Women’s Reproductive Health, 1(2), 138–152. https://doi.org/10.1080/23293691.2014.966597
Chrisler, J. C., Marván, M. L., Gorman, J. A., & Rossini, M. (2015). Body appreciation and attitudes toward menstruation. Body image, 12, 78–81. https://doi.org/10.1016/j.bodyim.2014.10.003
Cary, E., & Simpson, P. (2024). Premenstrual disorders and PMDD- a review. Best Practice & Research Clinical Endocrinology & Metabolism, 38(1). https://doi.org/10.1016/j.beem.2023.101858
Kulkarni, J., Leyden, O., Gavrilidis, E., Thew, C., & Thomas, E. H. X. (2022). The prevalence of early life trauma in premenstrual dysphoric disorder (PMDD). Psychiatry Research, 308, 114381. https://doi.org/10.1016/j.psychres.2021.114381
AbdelQadir, Y. H., Assar, A., Abdelghafar, Y. A., Kamal, M. A., Zaazouee, M. S., Elsayed, S. M., Ragab, K. M., Nabhan, A. E., Gamaleldin, N. A., Moris, M. S., AL-Masri, B. E., El-Sherif, D. M., Mohamed Goudy, Y., Khaled Alsiouty, A., Mahmoud, M. M., Faragalla, H. M., Abdelazim, E. A., Mohamed, N. A.-H., Elsayed, S. I., & Shehata, H. H. (2022). Prevalence and patterns of premenstrual disorders and possible association with sexual harassment: a cross-sectional study of young Arab women. BMC Women’s Health, 22(1). https://doi.org/10.1186/s12905-022-02130-0
Sattar, K. (2014). Epidemiology of Premenstrual Syndrome, A Systematic Review and Meta-Analysis Study. Journal of Clinical and Diagnostic Research, 8(2). https://doi.org/10.7860/jcdr/2014/8024.4021
The term “creative arts therapist” typically refers to someone who has a Master’s degree (or certification, in some countries) in one particular modality; they may also or only refer to themselves as a Drama Therapist, Art Therapist, Dance/Movement Therapist, etc. Expressive Arts Therapists study more than one modality of creative arts therapies, but often not as in-depth; they may focus on a few specific modalities but integrate them in a session. For example, a client may write a story and then make a drawing or act out parts. Both creative and expressive arts therapists study psychotherapy in addition to using the arts in therapy and there is no requirement to use art in every session or do any particular directives.
Saeideh Izadi Dehnavi, Seyede Salehe Mortazavi, Mohammad Arash Ramezani, Banafshe Gharraee, & Ashouri, A. (2024). Emotion-focused therapy for women with premenstrual dysphoric disorder: a randomized clinical controlled trial. BMC Psychiatry, 24(1). https://doi.org/10.1186/s12888-024-05681-8












this was great! thank you so much! i didn't want to stop reading, if you keep writing on this i'll be there first in line. x
Glad to find this resource. Thank you.