Cycling Through Chaos: Understanding the Intersection of Neurodiversity and Hormonal Health
The ADHD-PMDD Connection
Introduction
My first impulsive suicide attempt was around age 13, about a year after I got my first period. This is both my story and what science tells us about the complex relationship between ADHD and premenstrual disorders.
I was already depressed long before I got my period due to untreated ADHD and other unpleasant life circumstances. Still, if I look back at my high school and early twenty years, I seemed to be cycling through periods of passive depression and MEGA DEPRESSION or impulsive suicidality where I would ping-pong between parts that told me that I should kill myself before I lost my nerve to parts that were desperately looking for ways to hold on until the urge would pass.
I don’t remember ever being told I should track my cycle, that it could give me valuable information about my body and health. All my period was, was waiting until I got it and then having to deal with bleeding every month.
I was on various types of medications on and off since the age of 14: SSRIs, hormonal birth control, and stimulants. In my late 20s, I smoked a joint one night and realized I never felt like the meds were helping that much, so I decided to taper them off slowly (I saw a psychiatrist who advised me to do it over a few weeks. I ended up needing several months, as the withdrawal symptoms were so intense).
Recognizing Patterns
But I slowly started to notice patterns. Still, when I asked a psychiatrist if the meds I was taking could be making me feel rage towards my boyfriend before my period, he said no, that women who get PMS get worse as they age [my then on/off-again boyfriend was waiting for me outside and did not seem happy to hear this].
As my general mental health improved, it became obvious that my moods were tied to my cycle. I started tracking in various ways, slowly learning what was going on. It wasn’t easy, as the patterns changed over time, depending on factors in my life, including stress, diet, and exercise. Also, tracking something consistently long-term is a challenge with ADHD, and the fact that it’s still impossible to find a decent period-tracking app.
My Cycle Breakdown
Here’s how I described a recent cycle:
Day 1-3 of the cycle, feeling blah. I’m bleeding and achy and everything sucks. Then, I start getting more energy and motivation to do things. Climbing high, wanting to socialize, exercise, and take on new projects. I like men now! Until ovulation. Insomnia. Day 15, rage against the patriarchy, etc. This may last for a few days, but it’s less intense now that I’m allowing healthy space for anger (and all that woo-woo bullshit).
Day 24 - until whenever the fuck I start bleeding - doom and gloom or anxiety, moody, insomnia, physically exhausted, decreased focus, tender breasts, and/or acne. Depending on how bad my symptoms are, I’m on the couch with obsessive thoughts (I think this was around March when I experimented with a Concerta prescription) or I give myself time off to enjoy rewatching episodes of You’re the Worst (my last cycle).
I realized I needed to check where I was in my cycle because I wasn’t sure, and that’s a good sign I’m in follicular. I don’t feel the need to track when I’m feeling like I want to feel all the time—capable. But this time, I’m worried I’m taking on more than my luteal self can take, and I’ll crash.
The ADHD/PMDD Relationship: “It’s complicated”
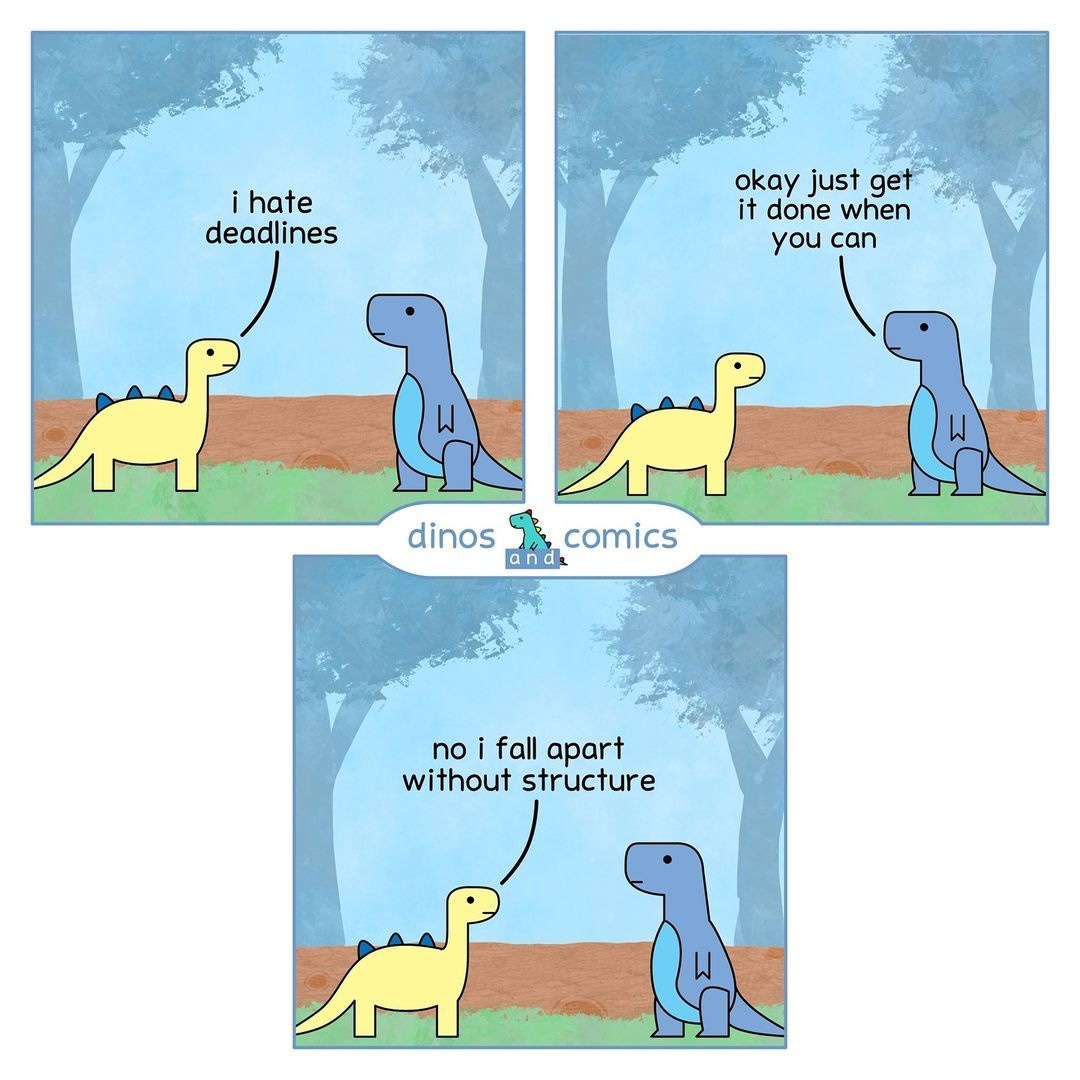
There are several unique challenges to managing ADHD and premenstrual disorders together. For one, ADHD makes it harder to plan for the future. So when we’re in a good follicular week, we can be tempted to believe that things are OK now, or we’ll simply forget to plan for luteal.
The inconsistency of ADHD and the inconsistency of premenstrual disorders feed each other. There’s personally a part of me that kind of thrives off the inconsistency and chaos, even as I hate it. I know routine can be great for me, but I hate that too.
Potential reasons for increased PMDD risk in ADHD individuals
Many women with ADHD report a premenstrual worsening of ADHD and depressive symptoms and seem to respond well to an increased psychostimulant dose in the week before menstruation1 (although many women describe feeling like the meds don’t work during luteal or make their PMS symptoms worse2). Additionally, there is a higher incidence of PMDD in women with ADHD.3
A study on adolescents found that those with PMS/PMDD scored lower on neuropsychological tests during their luteal periods - meaning they did less well on working memory and reaction times, visual-spatial and motor skills, verbal memory, attention, and concentration.4 ADHD seemed higher in the PMS/PMDD group but was not statistically significant. So even in women without ADHD, there are cognitive premenstrual symptoms. In women with ADHD, these common symptoms may be the tipping point of going from feeling functional to a non-functioning mess.
The research “suggests that PMDD perhaps has neurodevelopmental underpinnings (attention deficit hyperactive disorder, adverse childhood experiences) affecting the fronto-limbic circuit that regulates the emotions.”5
Trauma susceptibility and emotional dysregulation
People with ADHD are at an increased risk for trauma due to a host of reasons, including struggling with emotional regulation (meaning that it takes them longer to bounce back after a stressful event).
Symptoms of ADHD can correlate or be confused with temperamental dimensions, i.e., whether a child is born “easy,” “difficult,” or “slow to warm,”6 meaning that from a very young age, a child with ADHD may be labeled as difficult, lazy, or spoiled, leading to low self-esteem and depression.
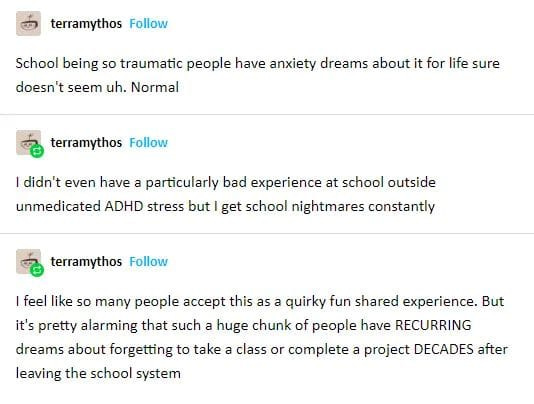
Trauma is a risk factor for PMDD7 as well. Children with ADHD may be more likely to experience maltreatment.8 For example, teachers and caretakers may react to a child who is hyperactive or distracted with increased control and punishments. The worse the child resists, the angrier the adults around them get, disrupting the relationship and creating a sense of failure in the child, who is often told that they’re not trying hard enough.
Increased sensitivity to internal sensations
Since women with PMDD don’t differ from women without PMDD in hormone levels9, the most accepted theory is that it is an increased sensitivity to hormonal fluctuations. ADHD and autism both involve increased sensitivity or reactivity.10
Recently, I noticed more of these “oh, something has changed” moments inside. There’s an internal resistance - nothing has changed in my circumstances, but my inner state has changed. This inner resistance seems to make my symptoms more extreme.
Potential BPA toxicity issues or food intolerances
People with ADHD may not clear BPA from plastics as efficiently, leading to an increased risk of toxicity. BPA is an endocrine disruptor that messes with a variety of hormones, including estrogen. And studies show that a drop in estrogen could affect working memory.11
People with ADHD may be more prone to food intolerance, such as soy, dairy, eggs, wheat, and corn12. When I read this, I did a food intolerance test13, which told me that I am intolerant to all of the above and several more. I have only been able to refrain from all the foods on my list for two weeks at a time, so I can’t report how much of a difference it makes on my symptoms, except that I use Bearable to track my symptoms and some foods. Indeed, there is a correlation between dairy, eggs, or soy consumption and some of my symptoms.
Untreated ADHD leads to other symptoms and disorders
Just like untreated PMDD can lead to other mental health issues such as depression and anxiety, the same goes for ADHD. Years of executive dysfunction lead to problems piling up, and self-esteem lowers, making it difficult to sustain healthy, supportive relationships and environments.
Many women experience some PMS symptoms, like decreased energy or increased moodiness, but these symptoms may be harder for women with ADHD to deal with, leading to worse consequences. For example, if a woman without ADHD can push through her exhaustion to do the dishes after coming home in her follicular phase, the ADHD executive dysfunction may make it harder with the PMS symptoms, leading to dishes piling up and a sense of overwhelm and failure.
Additional issues
The human body is complex, and there is a mountain of scientific literature. However, I can only cover so much in one article.
Further resources
There is increasing research, knowledge, and debate on how ADHD is different for women. In some cases, the line between “how ADHD looks in a woman” and “this is a hormonal sensitivity or premenstrual disorder” may be hard to draw. Reading/watching/listening to additional content on how hormonal fluctuations affect ADHD in women may be helpful.
ADHD and the menstrual cycle (comic/short article)
Women, ADHD, and hormones webinar
Jong, Wynchank, D., Esther van Andel, Beekman, A., & Kooij, S. (2023). Female-specific pharmacotherapy in ADHD: premenstrual adjustment of psychostimulant dosage. Frontiers in Psychiatry, 14. https://doi.org/10.3389/fpsyt.2023.1306194
I seem to be one of those women. Yay me.
Dorani, F., Bijlenga, D., Beekman, A. T. F., van Someren, E. J. W., & Kooij, K. (2021). Prevalence of hormone-related mood disorder symptoms in women with ADHD. Journal of Psychiatric Research, 133, 10–15. https://doi.org/10.1016/j.jpsychires.2020.12.005
Dorani, F., Bijlenga, D., Beekman , A. T. F., van Someren , E. J. W., & Kooij, J. J. S. (2021). Prevalence of hormone-related mood disorder symptoms in women with ADHD. Journal of Psychiatric Research, 133(133), 10–15. https://doi.org/10.1016/j.jpsychires.2020.12.005
S. Naik, S., Nidhi, Y., Kumar, K., & Grover, S. (2023). Diagnostic validity of premenstrual dysphoric disorder: revisited. Frontiers in Global Women’s Health, 4. https://doi.org/10.3389/fgwh.2023.1181583
Foley, M., McClowry, S., & F. Xavier Castellanos. (2008). The relationship between attention deficit hyperactivity disorder and child temperament. Journal of Applied Developmental Psychology, 29(2), 157–169. https://doi.org/10.1016/j.appdev.2007.12.005
Wittchen, H. U., Perkonigg, A., & Pfister, H. (2003). Trauma and PTSD - an overlooked pathogenic pathway for premenstrual dysphoric disorder?. Archives of women's mental health, 6(4), 293–297. https://doi.org/10.1007/s00737-003-0028-2
Craig, S. G., Bondi, B. C., O’Donnell, K. A., Pepler, D. J., & Weiss, M. D. (2020). ADHD and Exposure to Maltreatment in Children and Youth: a Systematic Review of the Past 10 Years. Current Psychiatry Reports, 22(12). https://doi.org/10.1007/s11920-020-01193-w
Cary, E., & Simpson, P. (2024). Premenstrual disorders and PMDD- a review. Best Practice & Research Clinical Endocrinology & Metabolism, 38(1). https://doi.org/10.1016/j.beem.2023.101858
Rossow, T., MacLennan, K., & Tavassoli, T. (2021). The relationship between sensory reactivity differences and mental health symptoms in preschool-age autistic children. Autism research : official journal of the International Society for Autism Research, 14(8), 1645–1657. https://doi.org/10.1002/aur.2525
Cobanoglu, C. (2021). The effects of PMS/PMDD on attention and shortterm memory in adolescent girls. Dusunen Adam:The Journal of Psychiatry and Neurological Sciences. https://doi.org/10.14744/dajpns.2021.00150
Stevens, L. J., Kuczek, T., Burgess, J. R., Hurt, E., & Arnold, L. E. (2011). Dietary sensitivities and ADHD symptoms: thirty-five years of research. Clinical pediatrics, 50(4), 279–293. https://doi.org/10.1177/0009922810384728
Although these tests are said not to be reliable. If I had the money, I’d like to do a similar test again to see if I get the same results. Interestingly, a friend told me they did a similar test and came out with zero sensitivities/intolerances.











This is great, very informative and I like that you used lots of research to back it up. I also wrote about ADHD and PMDD: https://neurodivergentnotes.substack.com/p/the-vicious-cycle-of-pmdd-and-audhd.